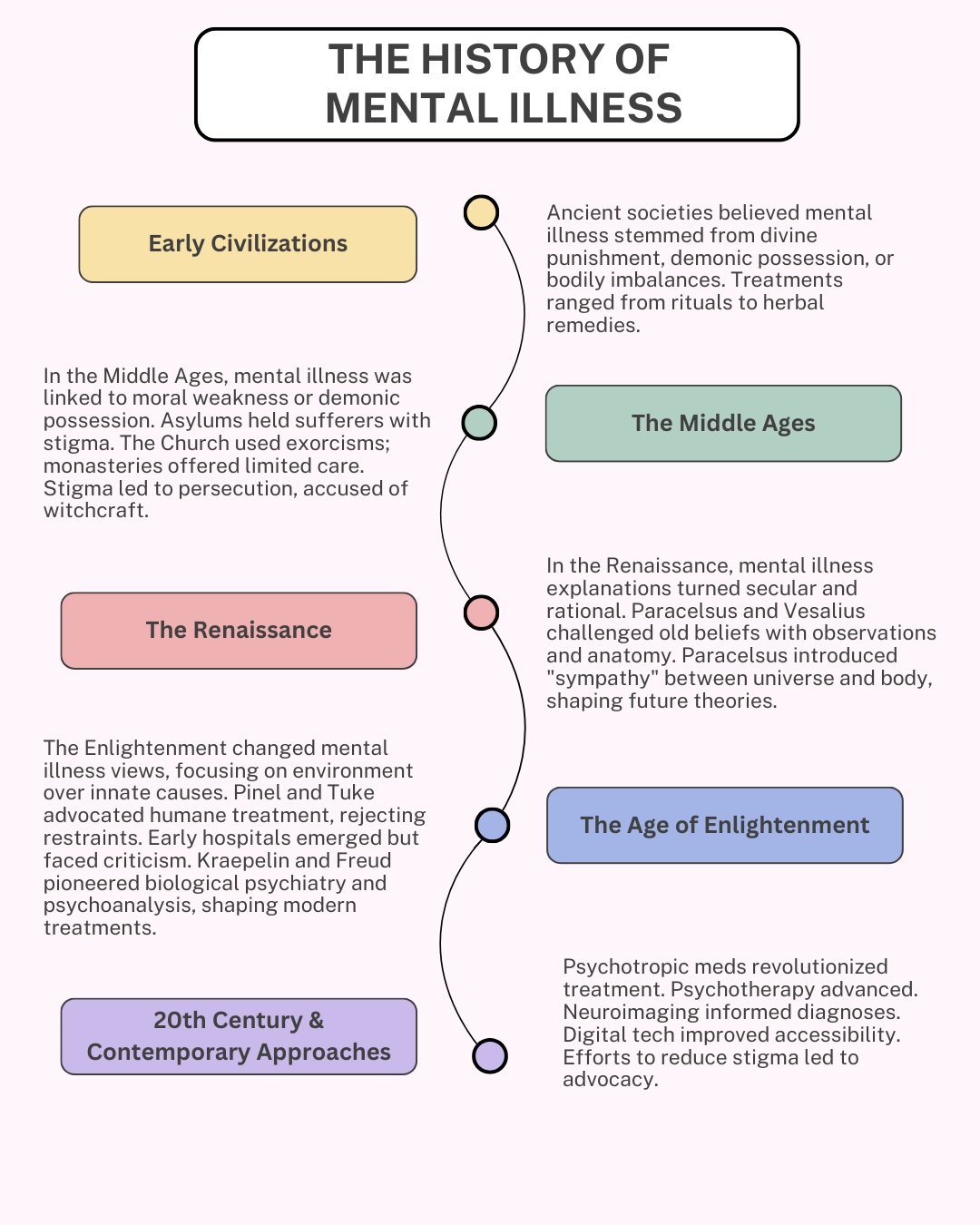
The history of mental illness is as old as human civilization itself, characterized by evolving understandings and treatments across cultures and time periods. From ancient rituals and superstitions to modern evidence-based interventions, the field of mental health care has evolved significantly, with each era contributing to our collective understanding of mental illness and its treatment. Understanding the evolution of attitudes, perceptions, and treatments surrounding mental health is crucial for comprehending contemporary approaches to mental well-being.
Early Civilizations
The earliest records of mental health date back to ancient civilizations such as Mesopotamia, China, India, Egypt, and Greece. Ancient texts reveal beliefs in demonic possession, divine punishment, or imbalances of bodily humors as explanations for abnormal behavior. Treatments varied widely, ranging from rituals, prayers, herbal remedies, and physical interventions aimed at restoring spiritual or physiological equilibrium. In Mesopotamia, where cuneiform tablets provided insight into medical practices, mental disorders were believed to be caused by divine punishment or demonic possession. Treatments involved herbal remedies made from plants like opium and mandrake, administered for sedative effects, and rituals performed by priests, such as prayers and offerings to appease gods or ward off evil spirits. Additionally, exorcisms and incantations were used to drive out evil spirits thought to cause madness. Similarly, in ancient Egypt, mental illness was believed to result from divine punishment or the displeasure of the gods, leading to rituals and magical spells as treatments. Furthermore, ancient Egyptian medical texts such as the Ebers Papyrus and the Edwin Smith Papyrus mention mental disorders like melancholia (depression) and hysteria (anxiety). These texts suggest a belief in both supernatural and naturalistic causes of mental illness. Treatments included herbal remedies, therapeutic baths, and rituals invoking the Gods, Thoth and Imhotep, for healing. Ancient Greek philosophers like Hippocrates proposed naturalistic explanations for mental disorders, emphasizing the importance of physical factors such as brain pathology and imbalances in bodily humors. Hippocrates, known as the father of medicine, rejected supernatural causes and instead attributed mental illness to imbalances in the four bodily humors (blood, phlegm, yellow bile, and black bile). Treatments aimed to restore balance through dietary changes, purging, bloodletting, and herbal remedies. Galen further developed these ideas, emphasizing the importance of lifestyle factors and environmental influences on mental health.
The Middle Ages, The Renaissance, and The Age of Enlightenment
During the Middle Ages, religious beliefs continued to shape understandings of mental illness. Mental health issues were often viewed as manifestations of moral weakness or possession by demons. Institutions known as “asylums” emerged, where individuals with mental disorders were confined, often subjected to harsh conditions and societal stigma. The Catholic Church viewed madness as a sign of moral failing or demonic possession, leading to practices like exorcisms and penance. Monastic communities provided some care for the mentally ill, offering prayer, confinement, and simple remedies such as herbal teas and poultices. However, stigma and fear often led to the marginalization or persecution of those with mental disorders, who were sometimes accused of witchcraft or heresy. The Renaissance saw a gradual shift towards more secular and rational explanations for mental illness. Figures like Paracelsus and Vesalius challenged traditional beliefs with empirical observations and anatomical studies. Paracelsus proposed the concept of “sympathy” between the macrocosm (universe) and microcosm (human body), influencing later theories of mental illness. The Age of Enlightenment also brought about significant changes in the perception of mental illness. Philosophers like John Locke emphasized the role of environmental factors in shaping human behavior, challenging prevailing notions of innate depravity or demonic possession. Figures like Philippe Pinel in France and William Tuke in England advocated for humane treatment and moral therapy, rejecting harsh methods like restraints and isolation in favor of compassionate care and social interaction. Pinel removed chains and restraints, introduced therapeutic activities and occupational therapy, and emphasized the importance of patient autonomy and dignity. The establishment of the first psychiatric hospitals in Europe marked a shift towards more systematic approaches to treating mental disorders. However, these institutions often lacked proper medical oversight and were criticized for inhumane practices. The rise of biological psychiatry in the late 19th century, led by figures like Emil Kraepelin and Sigmund Freud, introduced new theories of mental illness based on neurobiology and psychoanalysis. Kraepelin classified mental disorders based on clinical observation and the course of illness, laying the foundation for modern diagnostic systems. Freud explored the role of unconscious conflicts and early childhood experiences in shaping mental health, pioneering psychoanalytic therapy as a treatment for neurosis and hysteria.
20th Century & Contemporary Approaches
The 20th century heralded a revolution in the treatment of mental illness with the discovery and development of psychotropic medications. Lithium, first used as a treatment for mania in the 1940s, remains a cornerstone of mood stabilization therapy for bipolar disorder. The introduction of chlorpromazine in the 1950s marked the beginning of modern antipsychotic pharmacotherapy, providing relief for individuals with schizophrenia and other psychotic disorders. Subsequent decades saw the emergence of antidepressants, anxiolytics, mood stabilizers, and stimulants, offering targeted interventions for a range of psychiatric conditions. Advances in pharmacology and neuroscience have led to the development of second-generation antipsychotics, selective serotonin reuptake inhibitors (SSRIs), and other medications with improved efficacy and tolerability profiles. Psychotherapy, pioneered by figures like Freud, Jung, and Rogers, offered new avenues for understanding and treating mental disorders through talk therapy and behavioral interventions. Cognitive-behavioral therapy (CBT), developed in the 1960s by Aaron Beck, revolutionized the treatment of depression and anxiety by focusing on changing negative thought patterns and behaviors. Dialectical behavior therapy (DBT), developed by Marsha Linehan in the 1980s, has proven effective for treating borderline personality disorder and other complex mental health conditions. Advancements in neuroimaging technologies have provided unprecedented insights into the neurobiological underpinnings of mental illness. Functional magnetic resonance imaging (fMRI), positron emission tomography (PET), and electroencephalography (EEG) have allowed researchers to visualize brain structure and function in individuals with psychiatric disorders, informing diagnostic classification, treatment selection, and prognostic assessment. Neuroimaging studies have identified structural abnormalities, functional connectivity disruptions, and neurotransmitter dysregulation associated with conditions such as depression, schizophrenia, and post-traumatic stress disorder (PTSD). These findings have paved the way for the development of targeted interventions, including deep brain stimulation (DBS), transcranial magnetic stimulation (TMS), and neurofeedback, aimed at modulating neural circuitry and restoring brain health. The proliferation of digital technologies has transformed the delivery of mental health services, offering new opportunities for accessibility, convenience, and scalability. Telehealth platforms, mobile applications, and web-based interventions have facilitated remote consultations, psychoeducation, and self-management strategies, particularly in underserved or rural communities. Virtual reality (VR) therapy, biofeedback apps, and wearable devices have enabled innovative approaches to exposure therapy, stress reduction, and behavior tracking, enhancing user engagement and empowerment. Digital mental health interventions have demonstrated efficacy in reducing symptoms, improving functioning, and increasing treatment adherence across diverse populations, paving the way for expanded access to evidence-based care. In recent decades, there has been growing recognition of the global burden of mental illness and the need for concerted action to promote mental health equity and human rights. Additionally, efforts to reduce stigma and promote mental health awareness have led to greater societal acceptance and support for individuals living with mental illness. Public education campaigns, advocacy initiatives, and anti-stigma programs have helped challenge misconceptions and stereotypes, fostering empathy, understanding, and inclusivity. International initiatives such as the World Health Organization’s Mental Health Action Plan and the Movement for Global Mental Health have prioritized advocacy, capacity building, and policy reform to address disparities in access to care and social determinants of mental health. Efforts to destigmatize mental illness, promote community-based care, and integrate mental health into primary healthcare systems have gained traction, fostering collaboration and solidarity across borders. These initiatives underscore the importance of addressing social determinants of health, reducing inequalities, and promoting human rights principles in mental health policy and practice.
The history of mental health and mental illness is a complex tapestry woven from threads made of diverse cultural beliefs, scientific discoveries, and evolving social attitudes. From ancient beliefs in supernatural causes to modern neuroscience, from psychopharmacology to psychotherapy, and from neurobiology to digital health, the understanding, diagnosis, and treatment of mental disorders have evolved significantly over time. Historical approaches were often characterized by misunderstanding, fear, and mistreatment, and contemporary methods prioritize respect, dignity, and empowerment for individuals living with mental health conditions. Despite increased awareness and advocacy efforts, mental illness continues to be surrounded by stigma and discrimination, hindering individuals from seeking help and accessing appropriate care. Moreover, disparities in access to mental health services persist, particularly among marginalized communities, rural populations, and low-income individuals. Additionally, while advancements in psychopharmacology and psychotherapy have improved treatment outcomes for many, there is still a need for more targeted interventions, particularly for complex and treatment-resistant conditions. The integration of biological, psychological, and social approaches to mental health care remains a priority, as does the promotion of mental health literacy and the reduction of barriers to treatment. By addressing these challenges and continuing to innovate and collaborate, we can strive towards a future where mental health is prioritized, stigma is eliminated, and all individuals receive the support and care they deserve.